Dr. Eric Venn-Watson’s Highlights
Maybe your 5k pace is slower than it was last year. Maybe you’re feeling exhausted doing the same activities you used to perform without fatigue. Maybe you’re just wondering how to slow down the aging process so you can keep up with your kids and grandkids.
Whatever your reason, you’re reading this because you want to know how to live longer and age healthfully. Aging healthfully is a relatively new buzz term, although we’ve been chasing a way to stay youthful from a scientific standpoint for decades.
If we want to remain forever young, we’ll have to go back to the basics. This means talking about how our bodies function, what causes them to malfunction, and what we can do to prevent the eventual decline (here’s a hint: one little fatty acid that’s new to the game can be a game-changer).
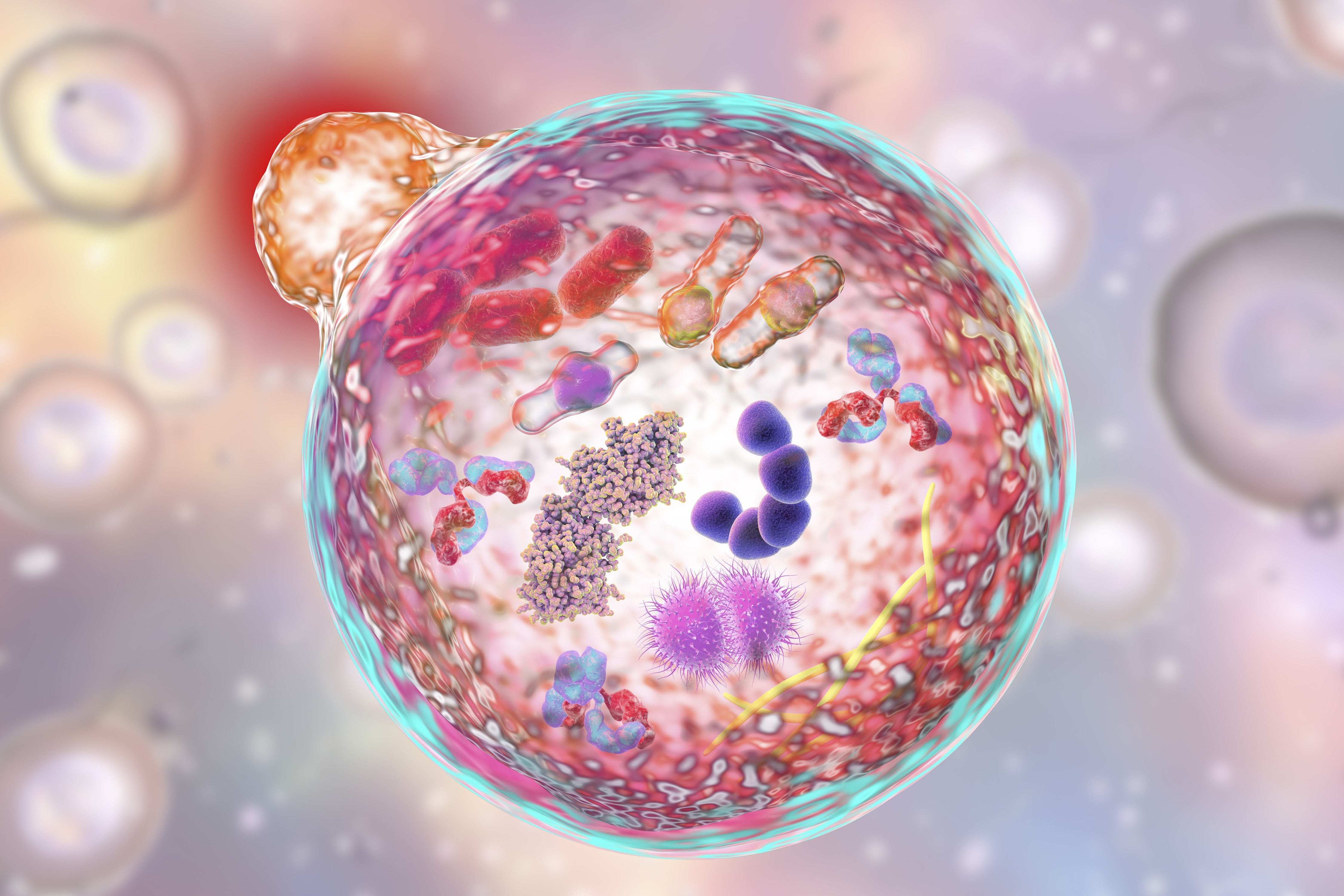
Cells 101
Beyond fad diets, new workout routines, and CoQ10 supplements lies an entire world of research about our cells. The foundation of every organ and system in our body is our cells, and discovering what keeps them healthy is the key to discovering what keeps us young.
Cells are responsible for building the tissues that create the organs that run entire systems and processes in your body. From an aging standpoint, it is essential that your cells function properly for as long as possible.
When your cells begin to lose function, it not only affects the way the tissues, organs, and systems in your body perform, it affects your very DNA.
When cellular DNA changes, cells begin to malfunction and replicate improperly, leading to malfunction, disease, and even death.
What Is Cellular Degradation?
Cells degrade. Just like a new car you drive off the lot, the degradation of your cells begins the second they are created and lasts until they eventually lose their function completely and die.
Obviously, this sounds like a grim situation, especially for the living beings we are. However, it’s important to remember that most cells are in a constant state of regeneration, meaning while some cells are dying, new cells are being created.
You’ve probably heard the rumor that the human body is essentially “replaced” every seven years. This is a clever concept with a seemingly sensible idea behind it. The rumor provides that because every cell in your body is in the process of regenerating and becoming a new cell, by seven years, your body basically replaces itself.
The problem with this idea is that, scientifically, it isn’t accurate. There are two main reasons:
Not all cells are capable of regeneration. Heart cells, for instance, aren’t regenerated, although they can be replaced by other types of cells. In addition, retinal cells are another example of cells that, once damaged, can’t be replaced. When these cells are gone, a portion of their function is lost, which could result in heart disease or vision loss.
Different cells regenerate at different times. Colon cells regenerate every four days. Skin cells take up to forty-five days. Skeletal bone cells take up to 15 years.
Because of those reasons, it’s impossible to have a completely new body every seven years. And because of cellular degradation, the cells that are new aren’t necessarily healthy, functioning cells like the ones you made when you were a child.
The Process of Cellular Degradation
Let’s get scientific about the specifics of how cells begin to degrade. When we consider the cell, we see that there has to be a balance between normal protein synthesis (necessary for cell function and structure), organelle biogenesis (the creation of new structures within the cell which carry out cellular function), and protein degradation (the use of new proteins by the cell) and organelle turnover (the process of dying cellular organs).
That means that while parts of the cell are dying and proteins are being used for functions, proteins need to be forming, and new organelles need to be created to replace the dying parts.
Cellular degradation occurs in two major degradation pathways: cellular autophagy and cytosolic turnover. Let’s look at what happens with each of these functions.
Cellular Autophagy
Autophagy is the way your cells clean house. This process of removing unusable cell parts and reusing usable parts keeps your cells healthy. Your cells contain autophagy-related proteins or ARPs. These are built by amino acids and cause autophagosomes to form within the cells. Autophagosomes act like garbage collectors, moving around the cell and collecting scrap parts.
The scraps are taken to organelles called lysosomes. These organelles are filled with enzymes that break down and digest the spare parts. The lysosomes then release usable parts back into the cell so the cell can recycle them.
Sometimes, extracellular material is brought into the cell through the plasma membrane. This material hangs out in the cytoplasm of the cell, where endosomes retrieve it. Endosomes sort the good from the bad and send the unusable materials to the lysosomes.
Autophagy happens when your cells are under stress. Numerous methods, including fasting and exercise, can induce stress. Stress can also be caused by disease.
Autophagy takes care of the balance of old and new organelles, and cytosolic turnover helps regulate the creation and use of proteins in the cell.
Cytosolic Turnover
Protein homeostasis is important to the health of your cells. Cytosolic turnover refers to the process of protein creation and degradation within the cell. It’s also sometimes referred to as protein turnover.
The main driver of protein synthesis is the concentration of mRNA transcript, a messenger molecule that helps a cell replicate its DNA. Protein degradation is driven by a process called the ubiquitin-proteasome pathway.
During this process, a protein called ubiquitin ligase (aka e3 ligase) that is loaded with ubiquitin tags a target proteinsubstrate that is not desirable or is no longer usable. Later, an enzyme called protease comes along and breaks these proteins down so they can be removed from the cell.
Both autophagy and protein turnover must remain balanced in the cell for it to remain fully functioning. When these systems fail, the cell may reach apoptosis.
Cellular Apoptosis
The process of cell death is known as apoptosis. The way your cells function is closely regulated by the body. When cells are no longer needed, they essentially self-destruct.
This might sound scary, but it’s a good and necessary biochemical process. Sometimes referred to as programmed cell death, apoptosis helps eliminate cells that aren’t needed during development, like cells between fingers and toes.
It’s also a major inhibitor of disease. Unusable cells are naturally eradicated through this process. If apoptosis does not occur, the inhibition of certain types of cells (like cancer cells) could lead to tumors.
However, as important as apoptosis is, too much of it can lead to neurodegenerative diseases, like Parkinson’s disease or Alzheimer’s.
The Bottom Line
Autophagic processes in the cell are necessary, but we need these processes to be balanced to avoid disease. You don’t need extensive knowledge of cellular biophysics to understand that an imbalance of degrading cells will affect the way we age.
The Effects of Degrading Cells
So let’s move away from the ligands, membrane proteins, and all the other bio-pharmacological jargon — how does cell degradation actually affect us?What we all normally think of as just normal parts of the aging process are really the result of our cells degrading. Bodies become slower, muscles become weaker, and bones become brittle.
But what about parts of aging that seem preventable?
It turns out, we can affect some age-influenced diseases and conditions like:
- High blood pressure
- Unhealthy cholesterol levels
- Weight gain, especially in the midsection
- Mental fog
- Insulin resistance
- General fatigue
These conditions may be somewhat preventable through activities like exercise, a balanced diet, and better self-care practices, but they’re also helped by better cellular healthcare, which, until now, has not been a primary focus for most of us.
Ultimately, cellular degradation is the underlying cause of cellular malfunctions, DNA changes within the cells, some diseases, and, ultimately, the death of healthy cells.
What Causes Cellular Degradation?
Once you know that cellular degradation exists, you’ll be on the quest to prevent it as much as you can.
Taking better care of yourself on a cellular level is referred to as practicing good cellular health.
Cellular health starts by identifying the different ways your cells may be degrading and eliminating as many of the causes of cellular degradation as possible.
Free Radical Damage
Free radical damage occurs naturally within the body but also happens because of external stressors that change the way your cells behave. Free radicals are unbalanced molecules that steal electrons from other molecules.
When the electrons are removed from healthy molecules, it damages the cell where the healthy molecule lives. This results in permanent damage that causes the cell to replicate incorrectly, malfunction, or even die.
Remember, when a cell in your body has been identified as damaged beyond repair or as unusable, it begins the process of programmed cell death. While some cells regenerate, not all do. So when cells die that do not regenerate, we’re left with a gap in our system.
Sources of free radicals include:
- UV rays from the sun
- Cigarette smoke
- Alcohol
- Pollution
- Some industrial cleaners
You can reduce the amount of free radicals that attack your cells by making healthier lifestyle choices and always limiting the amount of exposure you have to pollution and smog.
By loading up on antioxidants, you can also protect your cells from free radicals. Antioxidants work by donating one of their electrons to free radicals so that the cells are protected and safe. Antioxidants are found naturally in foods containing vitamins and certain fatty acids.
Poor Diet
Your cells need certain vitamins, nutrients, and acids to survive. To get these essentials, your cells look to your diet for nourishment. If you aren’t eating properly, your cells won’t have the essentials they need to function.
Over time, a lack of a balanced diet can have a negative impact on the life of your cells, causing them to degrade faster than they would if they received the proper nutrients needed for cellular survival.
The characterization of the standard American diet is a lack of fruits and vegetables and added sugar and trans fats that are unhealthy for our cells. These can leave the body depleted of nutrients and the cells in need of vital ingredients to carry out cellular functions.
Lack of Physical Activity
Physical exercise causes your cells to renew a bit faster. By damaging muscular protein cells through exercise, your body is triggered to create new cells. This may sound counterintuitive to the cause, but the type of damage caused to cells by exercise is healthy damage that lets your body know it’s time to renew.
Unlike the damage done by free radicals, which affects cellular DNA and causes cells to stop working properly, this type of damage causes cellular growth and repair through a natural process that your body needs to continue making new cells.
You need at least 150 minutes of cardiovascular activity per week and resistance training. Both of these types of exercises will help keep your body functioning properly and help your cells renew faster.
Practicing Better Cellular Health
Better cellular health is possible, but you’ll need to retrain the way you think about your health. Cellular health is more than just a balanced diet, occasional exercise, and a few word puzzles to keep your brain sharp. Recent science supports that maintaining our cellular health is the key component of our overall health and wellness. Further, science supports that a newly discovered as essential fatty acid, C15:0 (aka pentadecanoic acid) has the ability to improve our cellular health and even reverse cellular aging.*
Dr. Stephanie Venn-Watson discovered the potential benefits of C15:0 while working to improve the health and welfare of older dolphins. She initially found that the dolphins who were aging the most healthfully had higher levels of C15:0 in their diets.
Three years and multiple peer reviewed publications later, Dr. Venn-Watson and her team were able to show that C15:0 was an active and beneficial fatty acid that met the criteria of being the first essential fatty acid to be discovered in 90 years.
The team developed FA15™ to provide a sustainable, pure, and vegan-friendly source of C15:0 that was easy to take every day.
A variety of studies have shown that C15:0 improves cellular resilience, repairs mitochondrial function, and naturally targets PPAR receptors that regulate metabolism, immunity, mood, sleep, and appetite.
These studies also showed that daily C15:0 supplementation promoted healthy glucose and cholesterol levels, as well as healthy heart, liver and red blood cell function.
Since her first publication in Nature in 2020, there are now over 80 peer reviewed publications supporting the benefits of C15:0 to our overall health and wellness.
All in all, science supports that C15:0 is essential for our health.†
Elevate your cells. Elevate your self.
Buy NowWhy C15:0?
C15:0 helps support our cellular health in major ways:*
Supporting cell membranes. As we age, our cell membranes become more fragile. Cell membranes protect our cells from external stressors and help keep cells sturdy. When our cell membranes weaken, so do our cells' functionalities.
C15:0 is a sturdy, odd-chain, saturated fatty acid that integrates itself into cell membranes to fortify and strengthen them, giving them better protection against cellular degradation than omega-3 fatty acids, which allows cell membranes to become more fragile and susceptible to oxidative stress and cellular breakdown.
Increasing mitochondrial function. The mitochondria power our cells to carry out their functions, but cellular degradation causes the mitochondrial function to lead to impaired function of mitochondria, our powerhouses of the cell not generating as much energy for our cells.
C15:0 increases mitochondrial function by up to 45%, keeping our cells active and ensuring they’re able to carry out cellular processes as they should.
The mitochondria produce ATP, your cell’s energy currency. In studies, C15:0 was able to increase ATP by up to 350%. With more available cellular energy, C15:0 can help modulate cellular activity, giving it a boost.
C15:0 is also helpful in assisting with clearing damaged cells. C15:0 activates AMPK, an enzyme important to clearing away damaged cells. When there’s not enough of this enzyme, damaged cells may congest your system. AMPK helps regulate this process and keep the balance.
AMPK is also essential in regulatory processes, like glucose uptake. It also helps calm and lower inflammatory cytokines, which are known to be a key driver in premature aging.
C15:0 is essential for supporting your cells and improving your cellular health. Luckily, it’s really easy to get more of it in your body.
Fatty15 for Cellular Health
Because C15:0 is found primarily in trace amounts of whole-fat dairy products, your body may be deficient in this essential nutrientif you are not drinking whole-fat milk or eating other full-fat dairy products.
Additionally, many foods that naturally have trace levels of the good saturated fat, C15:0, also have lots of calories and much higher amounts of the "bad" saturated fats (like C16:0), which are associated with poorer health.
But that’s okay — fatty15 is the once-a-day supplement that offers you the pure, powder form, vegan-friendly, sustainably-produced, award-winning, version of C15:0, known as FA15™.
Just one fatty15 capsule per day gives your cells a fighting chance against the effects of cellular degradation.*
Get started with the fatty15 trial kit here, and see how simple it can be to support your health, look and feel better, and age on your own terms.*
Sources:
Interplay between metabolism and epigenetics: a nuclear adaptation to environmental changes|NCBI
Protein Degradation and the Pathologic Basis of Disease|Science Direct
Does The Human Body Replace Cells Every Seven Years?Live Science
Autophagy: Definition, Process, Fasting & Signs|My Cleveland Clinic.org
Autophagy as a Regulated Pathway of Cellular Degradation - NCBI.NLM.NIH.GOV/PubMed
Endogenous HMGB1 regulates autophagy
https://pubmed.ncbi.nlm.nih.gov/30065390/
Bibliography:
Chamberlain PP, D'Agostino LA, Ellis JM, et al. Evolution of Cereblon-Mediated Protein Degradation as a Therapeutic Modality. ACS Med Chem Lett. 2019;10(12):1592-1602. Published 2019 Nov 12. doi:10.1021/acsmedchemlett.9b00425
Chautan M, Chazal G, Cecconi F, Gruss P, Golstein P. Interdigital cell death can occur through a necrotic and caspase-independent pathway. Curr Biol. 1999;9(17):967-970. doi:10.1016/s0960-9822(99)80425-4
Harding TM, Hefner-Gravink A, Thumm M, Klionsky DJ. J. Biol. Chem. 1996; 271 :17621. [PubMed] [Google Scholar]
Klionsky DJ, Emr SD. Autophagy as a regulated pathway of cellular degradation. Science. 2000 Dec 1;290(5497):1717-21. doi: 10.1126/science.290.5497.1717. PMID: 11099404; PMCID: PMC2732363
Lemasters JJ, et al. Biochim. Biophys. Acta. 1998; 1366 :177. [PubMed] [Google Scholar]
Rousseau A, Bertolotti A. Regulation of proteasome assembly and activity in health and disease. Nat Rev Mol Cell Biol. 2018;19:697–712.
Tang D, Kang R, Livesey KM, Cheh CW, Farkas A, Loughran P, et al. Endogenous HMGB1 regulates autophagy. J Cell Biol. 2010;190:881–92.
Yan J, et al. Biochem. Biophys. Res. Commun. 1998; 246 :222. [PubMed] [Google Scholar]

Eric Venn-Watson M.D.
CEO, Co-Founder
Senior Scientist, Co-Founder
Eric is a physician, U.S. Navy veteran, and Co-founder and COO of Seraphina Therapeutics. Eric served over 25 years as a Navy and Marine Corps physician, working with the special forces community to improve their health and fitness. Seraphina Therapeutics is a health and wellness company dedicated to advancing global health through the discovery of essential fatty acids and micronutrient therapeutics.
You May Also Like...
2025 Longevity Review: Anti‑Aging Benefits of Fatty15’s C15:0
Introduction to Fatty15 and C15:0
Fatty15 represents a breakthrough in the field of longevity supplements, built around the discovery of C15:0 (pentadecanoic acid), an odd-chain saturated fatty acid newly recognized as essential for human health. Identified by researchers dedicated...
7 Supplements & Vitamins To Support Brain Health
Your brain is always “on.” It’s managing your thoughts, memories, moods, and internal monologue (which, let’s be honest, can get pretty lively).
Because it’s such a demanding organ, it needs consistent nourishment to keep neurons firing efficiently and communication networks...


