Dr. Eric Venn-Watson’s Highlights
Most adults know to get a regular cholesterol test every couple of years to make sure their hearts are healthy. However, new studies suggest that just a regular lipid panel measuring your low-density lipoprotein (LDL) and high-density lipoprotein (HDL) may not be the very best predictor of your risk of developing heart disease and stroke.
A team of researchers has studied a particular type of cholesterol (remnant cholesterol) and determined that, by itself, it might be a better indicator of your likelihood of developing heart-related issues. We’ll dive into the research, what it means, and what you can do to support healthy cholesterol levels.
First, let’s talk about what cholesterol is, and how it is measured.
What Is Cholesterol?
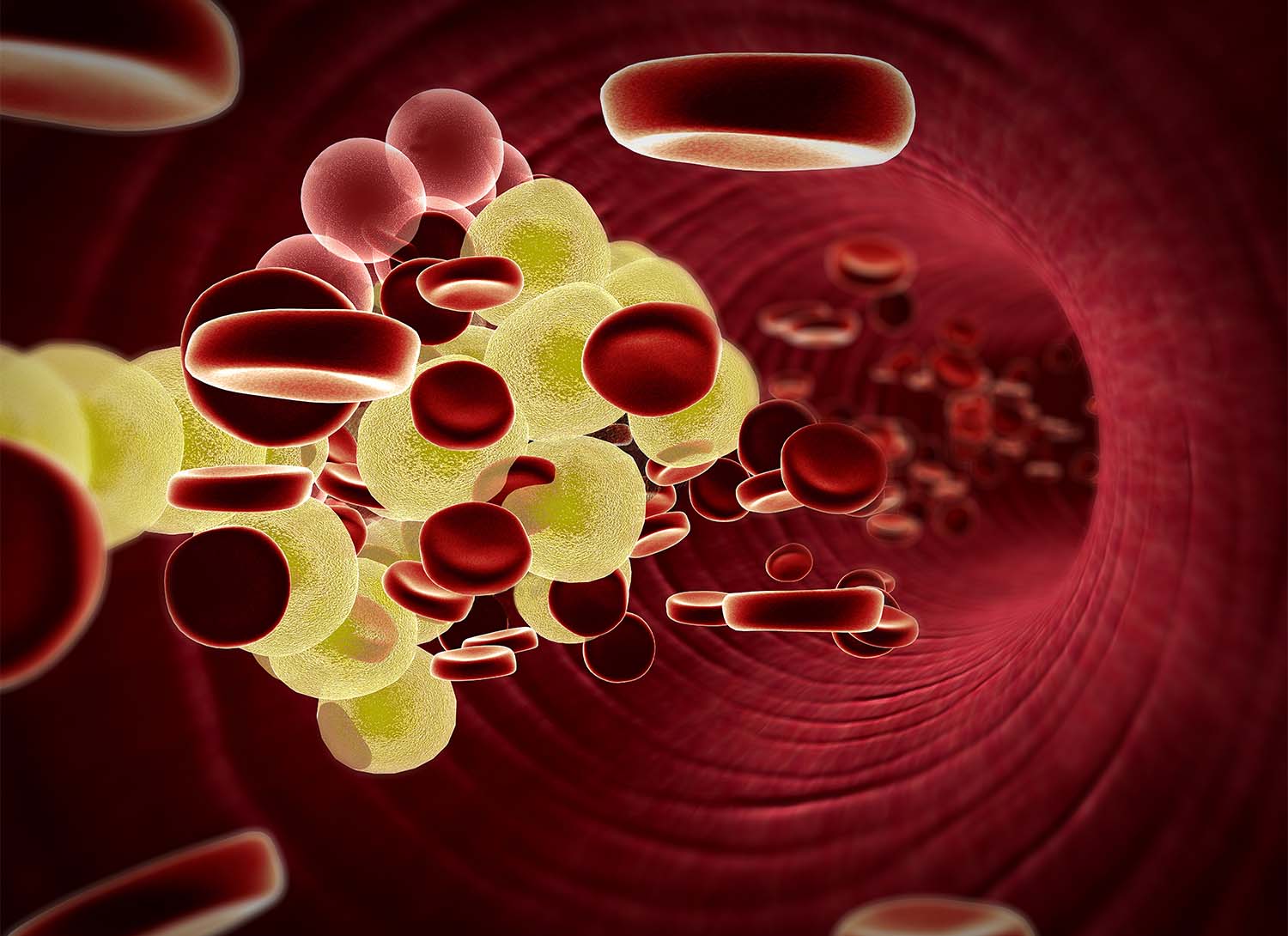
Cholesterol is a waxy substance that exists in your blood. It’s important and useful in many bodily processes right down to the cellular level, where it helps maintain cell membranes. However, too much of certain types of cholesterol are unhealthy and can lead to atherosclerosis, aka cholesterol buildup in the arteries.
How Is Cholesterol Measured?
Cholesterol is measured through a simple blood test. Usually, a person will be asked to fast for 10-12 hours before having blood drawn. The test is typically referred to as a lipid panel or lipid profile.
Cholesterol levels are measured in milligrams per deciliter. A lipid panel measures several different types of cholesterol.
-
Total cholesterol. Your total cholesterol measures your LDL, VLDL, and HDL cholesterol. This measurement should be lower than 200 mg/dL to be within a normal, healthy range.
-
LDL. Low-density lipoprotein cholesterol is also known as “bad” cholesterol. This type of cholesterol collects in your arteries and creates blockages. LDL cholesterol should remain between 100-129 mg/dL, according to general health recommendations, unless you have risk factors. If you have risk factors such as diabetes or heart disease, your LDL should be less than 100.
-
HDL. High-density lipoprotein is known as the “good” cholesterol. It can help lower the circulating levels of LDL cholesterol in your blood by transporting it to the liver, so having a level between 40-60 mg/dL is optimal. Generally, your HDL cholesterol should be above 40 mg/dL, and recent studies show that levels above 60 mg/dL may actually be considered too high.
-
VLDL. Very low-density lipoprotein is a type of LDL cholesterol, but one that carries triglycerides from your food into your bloodstream. This is also considered bad cholesterol because high triglycerides can also lead to heart disease and stroke. If you get a lipid panel, it will usually include a triglyceride reading.
-
Triglycerides. Triglycerides are not cholesterols, but fats. These are stored after your body converts the calories you need. A normal range is anything less than 150 milligrams per deciliter (mg/dL) with a high range of 200 to 499 mg/dL. Between these ranges is considered borderline, and should be paid attention to.
-
Non-HDL cholesterol. This measures your total cholesterol less your HDL cholesterol. Your doctor may pay close attention to this measurement, as it presents your combined LDL and V-LDL measurements.
These measurements give your healthcare provider a good snapshot of your heart health and allow them to evaluate your risk of developing heart disease. Additionally, recent studies suggest that measuring remnant cholesterol may provide more insight into your risk of heart disease and stroke.
Why Is Remnant Cholesterol Different?
Remnant cholesterol is calculated as total cholesterol minus LDL and HDL. Your remnant cholesterol reading measures the amount of “leftover” or remnant VLDL molecules excluding LDL and HDL.
This is more than just a measure of VLDL cholesterol because the VLDL measurement only measures VLDL cholesterol molecules before they take up triglycerides. The remnant cholesterol reading measures the VLDL molecules (including intermediate-density lipoprotein, chylomicrons, and their remnants) that have taken up triglycerides and delivered them to the bloodstream.
Why It Matters
For decades LDL cholesterol has been the most important marker of a person’s potential to develop heart disease and stroke.
However, studies of remnant cholesterol show that people with high remnant cholesterol numbers (over 24 mg/dL) are at a 40-50% higher risk of developing heart attack and stroke even if their LDL cholesterol numbers were within the normal or healthy range.
In other words, remnant cholesterol markers could be the key to early detection. Relying solely on LDL cholesterol readings may not be the best way to predict heart disease anymore.
For this reason, researchers hypothesize that remnant cholesterol is a better predictor of heart disease and stroke than LDL and total cholesterol readings.
What Else You Should Know
The research about remnant cholesterol isn’t limited to a higher probability of developing heart disease — while studying remnant cholesterol, researchers also discovered other correlations.
- People with higher remnant cholesterol were more likely to be obese. Obesity was linked to people with higher remnant cholesterol numbers, regardless of whether or not their LDL numbers were elevated.
- Higher remnant cholesterol numbers predicted type 2 diabetes. Of the study participants, people who developed type 2 diabetes had initial remnant cholesterol readings that were higher than participants who did not have elevated remnant cholesterol numbers. Again, this number was independent of their LDL number.
- Higher triglyceride levels were common with elevated remnant cholesterol numbers.
In short, remnant cholesterol may be the tool for helping to predict heart disease and stroke, serving as a crucial puzzle piece needed for early intervention.
Elevate your cells. Elevate your self.
Buy NowWhen It’s More Than Just Cholesterol
High cholesterol on its own is a problem, but other negative health markers may precede heart disease.
- Obesity. An increase in visceral fat, or fat that wraps around the midsection, is considered dangerous for cardiovascular health. This type of fat releases hormones that affect how your cells use glucose, and can affect your organs. Being overweight in general also places a higher strain on your heart, and can increase your risk of developing heart disease.
- Type 2 Diabetes. Unhealthy sugar levels from type 2 diabetes are most often attributed to lack of exercise and obesity. Type 2 diabetes also places you at a higher risk of developing heart disease.
- High Blood Pressure. Blood pressure measures the amount of pressure your blood pushes against your arterial walls. When your blood pressure is too high, your heart is working too hard to carry your blood throughout your body. This also places you at a greater risk of developing heart disease.
Together, these illnesses make up a condition known as metabolic syndrome. Individuals with metabolic syndrome are more likely to develop atherosclerosis, heart attack, and stroke.
To understand how these diseases affect our entire bodies, we need to look at our cells.
Cellular Health
We can boil down every system, organ, and tissue in our bodies to our cells. Our cells are the foundation of our beings, so it’s crucial that they remain healthy, especially as we age.
As we age, our cells naturally wear out. Cell membranes become weak, mitochondrial function declines, and cells lose the ability to communicate as well as they once could. This breakdown on the cellular level has a domino effect that contributes to illness and disease, especially regarding age-related diseases that may seem common and unavoidable.
Thankfully, they’re not unavoidable, and there is a solution for caring for our bodies on a cellular level.
Supporting Cellular Health
Supporting cellular health doesn’t take a degree in medicine or epidemiology, but a veterinary epidemiologist discovered a way to take care of our cells using a newly discovered essential fatty acid.
While helping dolphins live healthier lives, veterinary epidemiologist Dr. Stephanie Venn-Watson found that some geriatric dolphins had fewer age-related illnesses than other dolphins.
Dr. Venn-Watson found that higher circulating levels of C15:0, (which we now know is an essential fatty acid and the first to be discovered as essential since the discovery of omega-3s over 90 years ago) contributed to the health benefits that were seen in the healthiest dolphins. She went further, looking into the health benefits of this molecule in human populations, and three years later, published her findings in Nature's Scientific Reports in 2020.
C15:0 is an odd-chain, essential, saturated fatty acid that can reverse cellular aging, preventing our cells from premature breakdown. There are currently three known essential fatty acids, one type of omega-3, an omega-6, and now C15:0. While omega-3s have been linked to many health benefits, they are fragile and have a tendency towards oxidation due to their double bonds. C15:0, on the other hand, is a stable fatty acid that will not oxidize, allowing it to have a protective effect on our cells.
Because C15:0 is only found in trace amounts of whole-fat dairy products, some plants, and fish, there’s a good chance your circulating level of C15:0 is too low. As a population, we’ve avoided whole-fat products for over a generation. The increased switch to plant-based milks, which are deficient in C15:0, has also contributed to a global deficiency in C15:0.
Why can’t I just eat more foods with C15:0 you might ask. Simply increasing your intake of whole-fat dairy products comes with extra calories, sugars, and higher levels of the "bad" even-chain saturated fats. A solution? Pure C15:0 from fatty15.
How It Works
Fatty15 is the first and only supplement to the pure, vegan-friendly version of C15:0 known as FA15™. Just one capsule per day is enough to boost your circulating levels of C15:0.*
Fatty15 works in your cells in several significant ways:*
- Improved mitochondrial function. Sluggish mitochondria get a boost with 45% function increase.
- Cell membrane support. A sturdy fatty acid, C15:0 integrates itself into cell membranes to fortify them.
- Improved cellular signaling. By activating special receptors called PPARs, C15:0 helps bring back balance to functions like sleep, mood, appetite, and — surprise — cholesterol homeostasis.
Fatty15: Supporting Healthy Cells
Remnant cholesterol is a good tool to help your doctor determine your risk of developing heart disease. In the meantime, you can take care of your cells and ensure they’re able to function properly. Consider supplementing with fatty15 and give your cells a chance to age healthfully, resulting in a healthier-feeling you.*
Sources:

Eric Venn-Watson M.D.
CEO, Co-Founder
Senior Scientist, Co-Founder
Eric is a physician, U.S. Navy veteran, and Co-founder and COO of Seraphina Therapeutics. Eric served over 25 years as a Navy and Marine Corps physician, working with the special forces community to improve their health and fitness. Seraphina Therapeutics is a health and wellness company dedicated to advancing global health through the discovery of essential fatty acids and micronutrient therapeutics.
You May Also Like...
2025 Longevity Review: Anti‑Aging Benefits of Fatty15’s C15:0
Introduction to Fatty15 and C15:0
Fatty15 represents a breakthrough in the field of longevity supplements, built around the discovery of C15:0 (pentadecanoic acid), an odd-chain saturated fatty acid newly recognized as essential for human health. Identified by researchers dedicated...
The Ultimate Guide to Cellular Longevity Supplements for Optimal Health
Introduction to Cellular Longevity and Supplementation
Cellular longevity is the science of maintaining your cells’ optimal structure and function over time—a cornerstone for healthy aging and overall well-being. As we age, our cells face mounting stress, slower repair, and increased...


